Talking Back
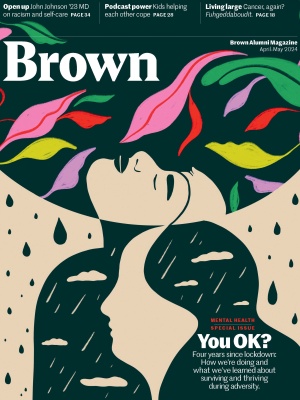
After the medical and racial nightmare that was 2020, John Johnson ’23 MD set out on a healing path that includes talking openly about mental health, racism, and medical disparities.
Summer 2020: in the wake of yet another police killing, it was not uncommon for John Johnson ’23 MD to wake up in a cold sweat in the middle of the night, thinking about racism.
At the time, the words to describe what he was feeling did not flow as eloquently as his reflections on race and mental health do now—rather, they hit him with an urgency that knocked him, quite literally, out of his sleep. Sometimes, he scribbled frantically into the opaque darkness. Other times, the words scribbled themselves onto the inside of his mind.
Johnson, then a second year medical student at Brown, was already used to thinking of himself and those around him as organisms: soft, fleshy entities whose every thought, feeling, and movement could be chalked up to a network of firing synapses nestled beneath the skin. But in these moments, Johnson found the tools of the scientist insufficient. He turned, as he has always done in desperate moments, to art.
“It often is a catharsis for me,” he says. “Almost like a way that I figure out how I feel about certain things.”
It was on one of those troubled nights that Johnson tumbled out of bed in the pre-dawn to scrawl the poem that would later become the inspiration for his photography collection exhibited on the first floor of the Warren Alpert Medical School building during the spring of 2021, “I Can’t Remember What I Yelled Back.”
The poem’s contents are brief and unambiguous. As for what readers should take away from it? Johnson says that, like the rest of his body of work, is open to interpretation.
“I love things being as loose as possible, as much room for interpretation… which is why I love creating ambiguous images,” he says. “Even if I don’t know what it means yet, or why it’s The Image, I know there’s something in there that is resonating heavily with me, and I have the rest of my life to figure out why that is.”
There is a persistent stigma among communities of color that “self-care” and “mental health” are for white people.
The Mississippi-born Harvard anesthesiology resident has spent most of his life cultivating a dual passion for medicine and art, but it was at Brown that Johnson would have his expectations for both of those fields violently disrupted—due in large part to the Covid pandemic, a global racial reckoning, and the intersection of these crises that upended everything he thought he knew about mental health. And, as so many in the medical field did in that time, Johnson chose to run toward, not away from: toward the hard conversations and painful reflections and, ultimately, toward the most delicate parts of himself.
“I remember telling my dad, a lot of times in my life, I just felt like I was running full speed with my eyes closed—trying as hard as I could, but not necessarily knowing what was coming next,” he says. “But I haven’t hit a wall yet, so I’m just gonna keep running.”
Along the way, he would find his artwork exhibited in a Providence barbershop and create a mental health screening tool to assess the psychological needs of other aspiring doctors that has since been incorporated into Brown’s medical school curriculum. At Mass General Hospital, Johnson prides himself on being a reassuring presence to the Black families who often come with reservations about whether they will receive the same world class healthcare promised to their white counterparts. And in Boston, in between the 14-hour shifts, Johnson hits the gym and thinks about his next picture or poem, grateful that these days he mostly sleeps through the night.
One night after a high school basketball game,
I was standing outside the school with two of my friends,
and on a distant offroad, five to six white children yelled, “Niggers!”
I can’t remember what I yelled back.
“That poem was a microcosm of what so many Black Americans have to deal with in this country,” Johnson said in a companion video about his photography collection, filmed by one of his peers in 2021. “It’s people being so hateful toward us, knowing that there won’t be any repercussions for their hate.”
Racism and illness
Those who do feel the repercussions, however, are the victims of racial hate, especially Black and Indigenous citizens who bear the brunt of racism’s physical toll. Even beyond the more obvious acts of civilian and police brutality, research indicates that Black people also experience the country’s highest maternal mortality rates and have a shorter lifespan than white Americans, regardless of socioeconomic status.

The racial disparities that have long been present in healthcare were dragged into the limelight once again at the outset of the pandemic, when at one point Black people had the highest Covid mortality rate of any ethnic group in the country, more than double that of white Americans. (Indigenous Americans also experienced disproportionately high mortality rates during the early stages of the pandemic.)
While misinformation was a key factor in the early spread of the virus, research also quickly emerged pointing to the high prevalence of comorbidities among Black Americans: pre-existing health conditions such as asthma, diabetes, or heart disease, often the result of inadequate or infrequent access to healthcare, that increase a person’s vulnerability to the virus and likelihood of hospitalization.
In the four years since Covid first touched down in the United States, Black Americans have become increasingly vocal about the impact of structural racism on their health, whether it’s the severely underfunded community health center in their neighborhood, the doctor who refuses to listen when they complain of chest pain, or the waste management facility down the block spewing fumes onto their elementary school playgrounds.
Where there is still some hesitation, however, is when it comes to the quiet killers: the noisy late-night entrance that reeks of whiskey, the missing pill bottles, the silent dinner tables that refuse to say the word suicide. There is a persistent stigma among communities of color that “self-care” and “mental health” are for white people—a stigma that is being slowly dismantled but still tightly grips many minority communities like the one that raised Johnson in Greenville, Mississippi.
“I think the biggest part is just the normalization of it… like if someone says that they go to therapy,” Johnson says, people should feel empowered to respond by saying: “Nice. I’m happy that you’re engaging in it.”
The desire to increase conversations about mental health drove Johnson to create a survey and resource guide as part of a project during his family medicine rotation at Brown, with the hope of helping his peers identify their mental health needs and steering them toward the kind of support he wished he’d known to ask for sooner.
“I couldn’t go anywhere because of the pandemic, but I was also afraid to go outside because of the racial tensions.”
“We’re well aware how much pressure people are put under in medicine. We’re well aware that people deal with anxiety and depression and even different substances,” he explains. “And even if people decide that they don’t want to take the survey, by offering it at every rotation, it means mental health is at least thought about, and at least we’re talking about it.”
Panic during Covid
Just after 5 p.m. on an afternoon in May 2020, Johnson’s vision started to go black.
It was the evening before the rheumatology exam and the first-year medical school student was on his third pass over the roughly two dozen lectures he had to commit to memory by 9 the following morning. This was how he always studied, and yet suddenly, as he looked at the slides through glazed eyes, his brain seemed to empty itself of everything.
“I was like, I don’t remember any of this information,” he recalls. “It was almost like it was the first time I was seeing it.”
He stared and stared, but his mind retained nothing. Instead, he began to feel the weight of all his body’s unmet needs. He was running on just a few hours of sleep. He had eaten only a piece of toast with peanut butter. And, of course, thoughts of George Floyd and Ahmaud Arbery’s brutal killings were never far from his periphery. Without his consent, his brain resolved that it could go no further and sounded the panic alarm.
“I felt everything closing in, I was breathing really heavy,” he remembers. The next thing he knew, he was on the floor of his Providence apartment. “It was intense… I couldn’t go anywhere because of the pandemic, but I was also afraid to go outside because of the racial tensions and things, so it was sort of like this pressure cooker.”
When he was finally able to think—and see—clearly again, he called his mom and followed her sage advice to eat some real food and go to sleep. Ultimately, he scored just shy of a 90 on the exam, but it was the experience of that night, and not the lengthy list of musculoskeletal diseases, that stayed with him throughout medical school and into his residency.
“It was one of the strangest, scariest moments of my life,” he says. “That was the birth of me taking care of myself.

Although he had never experienced an acute panic attack before, Johnson said the moment forced him to come to terms with ongoing patterns of anxiety that had tried to surface over the years but had largely gone ignored.
“Even when I was in college, there would be times where I would just be walking through the mall by myself and I would become so anxious that I would just leave the mall. And that didn’t strike me as strange back then, that’s just how I was,” he recalls. “But as medical school and being in medicine often does, it forces you to face whatever thing that you haven’t faced. So I’ve started becoming more intentional about taking care of my mental health.”
A core part of Johnson’s self-care routine is exercise: challenging his body with strength and resistance training. But equally important, he says, is communication, and challenging himself emotionally to open up to others.
“It’s inspired me to be vulnerable with other people and myself. Acknowledging that, okay, you’re really anxious right now. Don’t act like you’re not anxious. Don’t be afraid to tell people what you’re feeling,” he says.
Where he might once have been reluctant to name his negative emotions or even bother figuring out what he’s feeling, Johnson says he’s now “super honest” with family and friends.
“Sometimes it makes my momma nervous, because I think I tell her too much,” he adds, laughing, “but it’s like, I tell her when I feel it so that it doesn’t build and then come out in a crazy way.”
Another crucial component of Johnson’s self-care is, of course, his artwork. Beautifully illustrated in the collection he presented at the Alpert Medical School in 2021, I Can’t Remember What I Yelled Back is something of a master class in the use of photography to process difficult emotions.
The pictures offer an intimate look at very real people, both distant and familiar, who endure and resist the impact of racial inequality in quiet ways every day.
The exhibit was born in 2020 out of a desire to respond to the explosive national debate over racial justice with a deeply personal reflection on the people closest to him. The photos of Johnson’s family and community members from his hometown of Greenville sought to peel away from stereotypes or caricatures of Black people that a viewer might be tempted to conjure in their head. Instead, the pictures offer an intimate look at very real people, both distant and familiar, who endure and resist the impact of racial inequality in quiet ways every day.
“That whole project was a catharsis, because I was just so overwhelmed,” he said. “Photography was the way that I got all of those emotions out.”
Johnson brought the collection to Providence after showings at the Columbus Arts Council, the Mississippi Museum of Art, and his undergraduate alma mater, Tougaloo College, but says one of his proudest moments was having a few of the pieces displayed in a local Providence barbershop after meeting one of the barbers at a mobile vaccination clinic.
“When they were in that Black barbershop, they looked more at home,” he explains. “They just blended in and added to the environment, versus when they were in a museum, they looked like something that was supposed to be observed and evaluated.”
But Johnson sees the value in displaying his art in a range of locations—and hopes to expand the collection to include a sound installation in the coming year. Wherever the exhibit hangs, he’s proud to know it’s driving the conversation on racial equity forward, whether the viewer appreciates it or not.
“To future physicians, patient perspectives are not optional. Presenting these photographs on the first floor means the viewer must engage with this perspective in one way or another,” he wrote in his artist’s statement for the Alpert Medical School’s exhibition. “Whether that engagement be through careful consideration or by completely neglecting it, both scenarios are equally important.”
Acknowledging the elephants
Even as the newest person on his team at Mass General, Johnson doesn’t doubt his value—it’s reinforced every day as he helps his coworkers bridge the gap between their own experience and their patients to provide reliable, supportive healthcare to communities of color.
“When we have Black patients, as we’re telling them the plan, a lot of times they’re looking right at me, kind of like, ‘You agree with this? Is this okay? Are they telling me the truth?’” he says. “It’s important that people have that.”

Although there’s still a long way to go, Johnson believes the medical field has learned a few lessons from Covid on the importance of connecting with minority communities and about what good public health communication looks like. Though not everyone wants to admit it, outreach starts with recognizing the racism lurking in our systems: our clinics, pharmacies, and hospitals.
“There are these internal biases that you always have to be fighting against and improving upon,” he says, “and I am huge on acknowledging elephants within the room.”
While much of that work is introspective, Johnson also encourages his peers in medicine to give patients the opportunity to share when a racial, ethnic, or language barrier is diminishing the quality of their care, or damaging their trust in the healthcare system.
It might be as simple as giving a patient a chance to say, “Hey, I’m uncomfortable. There are four doctors who do not look like me. Maybe they don’t even speak my language and they’re telling me what’s wrong with me and what we need to do,’” Johnson suggests. “But the baseline is acknowledging what everybody’s thinking about so we can get that tension out of the room and focus on your health.”
Though a return home to Mississippi after medical school once seemed enticing, Johnson’s experience as a visiting student at Brown during his time as a Tougaloo undergraduate has ignited a desire to launch a pipeline program to guide aspiring high school students from his hometown into college, and all the way to Harvard Medical School, if they choose.
“Where I come from, the Mississippi Delta, so many of my classmates and people in my community were as smart as me, often smarter than me, but they just didn’t have the resources,” he explains. “Ultimately all of that potential they had, for lack of better words, died in the city where we were born. And to me, that sort of thing is unacceptable.”
On a mission to “reach back” to his community and pull them forward, Johnson hopes to model not only an empathetic approach to medicine but also a steady practice of self-care that is rooted in equal parts introspection and communication. And while he knows building those rhythms might be uncomfortable, Johnson isn’t afraid to ask the hard questions and say the vulnerable things and run, run, run toward a future that’s brighter for everyone.
Ivy Scott ’21.5, a CASE and Eddie award–winning former BAM intern, is a climate reporter at the Boston Globe.