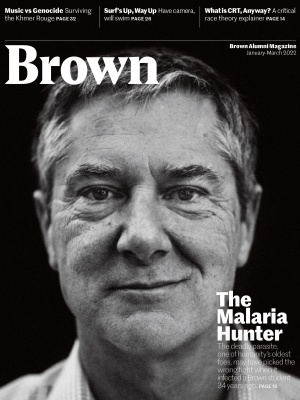
The Malaria Hunter
A Brown pathology professor may have developed a revolutionary new approach to battling one of the world’s deadliest diseases

Jonathan “Jake” Kurtis was riding a night train from Nairobi to Mombasa when he first began to feel sick. Then a 20-year-old Brown junior, Kurtis had gone to the restaurant car for a curry and stayed up late drinking beer with some Americans he’d met. By the time he got back to his sleeper car, he had a vicious headache. “I thought God had visited upon me a righteous hangover,” says Kurtis, speaking from his office at Brown, where he’s now a professor of pathology and laboratory medicine (he graduated with the class of ’89 and then stayed for a PhD in pathobiology in ’95 and a medical degree in ’96).
By the time Kurtis got to the Kenyan coast he was suffering from vomiting and diarrhea, too weak even to carry his rucksack. Somehow he got to a little mud hut he had rented on the beach. “At that point, I don’t have any memory for about three days,” he says. When he came to, he spied three open foil packets by the side of his bed. They’d contained tablets from a travel doctor to take in case of fever—taking them in his delirium may have saved his life.
Kurtis came to see the experience as a blessing. “I was lucky enough to get cerebral malaria,” he says. The disease has a fatality rate of 28 percent and can cause lifelong brain damage in survivors, who may also contract the disease multiple times during childhood, making them listless and feverish during crucial developmental years. It altered Kurtis’s life in a different way, inspiring him to devote his life to eradicating it.
Dressed in a black V-neck T-shirt and sporting tousled salt-and-pepper hair, Kurtis has an irreverent sense of humor and an easygoing bedside manner that is rare for a scientist. But he turns passionately serious when talking about one of Africa’s deadliest diseases. “I had a real epiphany, which is that malaria is a great thumb keeping the population of much of the world depressed,” says Kurtis. Approximately half a million people die every year from mosquito-borne illness, about half of them young children living in sub-Saharan Africa—one child every 2 minutes. “When you have a quarter of your children under the age of five dying, it’s unsustainable as a society.”

Malaria is a formidable foe (see the “Life Cycle of a Serial Killer” sidebar below), and to date no vaccine has succeeded in completely eradicating it from the body. This past October, the World Health Organization recommended a new vaccine called RTS,S/AS01, or Mosquirix, which it hailed as a breakthrough. Even so, trials in African countries demonstrate that the four required doses show at best 30 percent efficacy after four years—and offer close to no protective effect after that. Compare that to studies showing that insecticide-coated bed nets reduce malaria cases by 41 to 56 percent.
As fearsome a disease as malaria is, it’s long been hypothesized that some children are naturally immune. To a young Kurtis, this seemed the key to the development of a radically different kind of vaccine that might stop malaria altogether, and he’s been working to unlock the mystery ever since.
A fateful escape from the Open Curriculum
Before his transformative junior year abroad, Kurtis grew up in Portsmouth, Rhode Island, a half-hour down Narragansett Bay from Providence, attending the Catholic high school Portsmouth Abbey. He always loved science—“loved, loved, loved it,” he says. But after his strict high school experience, he felt overwhelmed by Brown’s famously flexible curriculum. “If you’re intellectually self-actualized, there’s nothing better than a school that gets out of your way,” he says. “But if you are used to running in the narrow gauge of a parochial high school, you feel like you are running off the rails.”
So when a friend returned from a cultural immersion program in Kenya, he followed suit: “I didn’t know what to do—but thought it’d be fun to think about what I wanted to do while doing that.” His project was an eight-week research project on coral reef ecology, but after his brush with cerebral malaria he switched focus to biology and earned a spot at Brown’s Warren Alpert Medical School. He had figured his quickest path to treating disease was to become a doctor—but after finding he wouldn’t be able to conduct scientific research, he regretted the decision: “I hated it!”
“I had a real epiphany, which is that malaria is a great thumb keeping the population of much of the world depressed.”
He met with his mentor, Richard Olds, director of the International Health Institute (and the same doctor who’d given him the malaria pills for Kenya) to tell him he was quitting. “He said, are you out of your mind? Don’t quit—double down!” Olds convinced Kurtis to switch to a joint MD-PhD program so he could earn his medical degree while conducting microbiology research.
Joining Olds’s lab, Kurtis focused on schistosomiasis—“schisto” for short—an intestinal disease caused by a parasitic flatworm. There he met his future wife, Jen Freidman ’92, ’96 MD, now a professor of pediatrics and epidemiology at Brown. Post doctorate, he got a research grant from Walter Reed National Military Medical Center to return to Kenya and help with early tests of the RTS,S vaccine, which the U.S. military was interested in for soldiers overseas. At the same time, Friedman got a Fulbright to work in Kenya with the Centers for Disease Control. In 1996, they got on a plane together to fly to Kisumu, a small city on Lake Victoria. It was a seminal year for them both. Driving between villages in a pickup truck, Kurtis came face-to-face with the ravages of malaria, treating children suffering from fevers or sitting listless inside their homes. The RTS,S vaccine he was testing attacks a key protein in the early stage of the disease but wasn’t showing much promise in giving immunity. While in the field, however, Kurtis had time to pursue his own idea for finding an antibody.
Kurtis had gotten the idea while at Brown, based on the work of a professor on his thesis committee, Paul Knopf. Working on schisto, Knopf investigated the response to the disease in two different kinds of rats. “Both rats made antibodies, but only one made the critical antibody that granted protection,” Kurtis says. In an effort to understand why, Knopf overlaid the genomes of the two species like a Venn diagram. They overlapped almost perfectly—with only a few exceptions. Those differences, he concluded, must be what gave one variety of rats immunity. He used this information to create a new vaccine that succeeded in immunizing rats from the disease.
In Kenya, Kurtis set out to apply the same principle. As he took blood samples from children, he noted that some seemed particularly susceptible to malaria, given the number of times they’d gotten the disease; others seemed resistant. If he could isolate the differences, he thought, maybe he could isolate protective factors that convey immunity.

Of course, children aren’t lab rats—and there were an endless variety of factors that could influence who got sick. As he took his samples, Kurtis asked questions about the children’s living situations—who lived near bodies of water that bred mosquitoes, who slept under bed nets—in an attempt to weed out reasons for their resistance or susceptibility.
“Jake’s background in basic science and his ability to apply that to populations sets him apart from other researchers,” says Chandy John, a professor of pediatric infectious diseases at Indiana University who specializes in malaria. “Unlike many of us who have a clinical background only, he has a sturdy PhD background so he can understand these basic mechanisms that might lead to protection.”
Getting malaria to kill itself
After the second stint in Kenya, Kurtis did his residency and fellowship at the University of Pennsylvania before returning to Brown as an assistant professor in 2000. He set out to analyze the blood serum he’d collected from the kids in Kenya with the help of Chris Nixon ’05 GS, ’08 MD. After controlling for confounding factors, they chose ten children who seemed most resistant and ten who seemed most susceptible, then performed a differential screening to analyze their differences.
While they came up with some interesting hits, nothing seemed definitive. Rather than give up, they applied their learning to a new set of pediatric serum samples collected by Patrick Duffy—Kurtis’s supervisor on the Kenya project—a few years later in an effort funded by the Gates Foundation. Duffy is now chief of malaria immunology and vaccinology at the National Institute of Allergy and Infectious Diseases (NIAID). This time, Kurtis and Nixon recorded even more characteristics to better identify those children most apt to hold protective factors. “He really has an unbelievable persistence,” says Nixon, who was by then a resident at UCSF. “A lot of things didn’t work, but he kept pushing and really wouldn’t take no for an answer.”
“A lot of things didn’t work, but he kept pushing, and really wouldn’t take no for an answer.”
By now, they were aided in their pursuit by Dipak Raj, an assistant professor of pathology at Brown, who had come up with a similar idea based on his studies of malaria in India. Friedman, meanwhile, performed the data analytics for the project. “We always joke that we are each other’s best collaborators,” she says. “We work well together without getting frustrated.” This time, they had a breakthrough—a protein in the resistant children’s serum that when injected into mice seemed to confer immunity from malaria.
When they analyzed the cells of the immunized mice, they made an amazing discovery. The antibodies did not attach directly to the malaria parasites. Instead, they attached to the outer wall of the red blood cells after they were already infected by the pathogen, building a protective wall that prevented the schizonts (see sidebar) from breaking out of the cell to infect new cells. “Once they are trapped, they don’t get out, they don’t multiply,” says Kurtis. “It’s like being trapped inside a burning house.”
The team called the protein they discovered schizont egress antigen (SEA). They were elated to have found a completely new way to fight malaria. “Instead of a sterilizing immunity, where you clear 100 percent of the parasite from the bloodstream, you could still be walking around with a million parasites in your blood cells—but you no longer get sick,” says Nixon. “It’s amazing.”

The team wrote up their findings in a paper published in 2014 in Science, then moved on to testing other proteins—and discovered another antigen that seemed to confer immunity, which Kurtis and Raj christened “glutamic-acid-rich protein” or GARP. This protein also affected the parasite while inside red blood cells. In this case, however, instead of just trapping it, it seemed to somehow send a signal to the parasite to initiate a controlled cell death called apoptosis. “It actually kills itself,” Kurtis says.
He hypothesizes the phenomenon is part of an evolutionary process in which malaria developed an ability to keep from killing its host while it multiplied to its maximum amount. Whatever the reason, the discovery of this “kill switch” promised yet another new approach to containing and destroying the malaria parasite.
It was one thing to show the vaccine worked in mice, however, and another to show it could work in humans. In an effort to get one step closer to proving its effectiveness, Kurtis and Raj decided to go for broke by commissioning a trial in monkeys to see if GARP would provide the same kind of immunity. “They are a quarter of a million bucks, and it was all the money I had—I was taking a leap of faith,” Kurtis admits. They commissioned a study with a Maryland-based company, and initial results seemed positive. At that point they decided to try another trial, only instead of using a traditional vaccine using recombinant protein they used a new technology for vaccine delivery called liquid encapsulated mRNA—the same technology used by Moderna and Pfizer to create a vaccine for COVID-19.
The results were promising. After being exposed to malaria, control monkeys that had not been vaccinated developed parasite levels three and a half times that of the vaccinated monkeys. Furthermore, of the five monkeys that were vaccinated, only two reached levels of malaria infection that required treatment after 16 days, while all four control monkeys needed treatment after 13 days.
“The data was exactly what we would dream for,” says Raj—direct evidence that the vaccine helped to confer immunity in non-human primates. They wrote up a new paper, published in Nature in April 2020. “The animal data is extremely promising, showing that this approach is working,” says the NIAID’s Duffy. “Jake has provided evidence that this is a very promising target, and the next step is to target human studies.”
Sending grant applications into the void
Kurtis imagines combining SEA and GARP to trap the parasites in the cell, then make them kill themselves. They could be further combined with a vaccine targeting the sporozoite stage such as RTS,S. Nixon, meanwhile, is working on a vaccine that kills the gametocytes that go on to infect new mosquitoes and could help curb malaria’s spread.
There is one thing holding Kurtis back: money. Unlike diseases such as cancer, heart disease, or HIV/AIDS, malaria is exclusively a disease of the developing world, so government funds to combat it are scarce. “All the major funding agencies are in wealthy countries, so they respond to their own constituents,” says Indiana University’s John. “If malaria were more of a problem in the United States, there’d be a lot more support for research.”
Without an effective vaccine, malaria’s unrelenting toll dwarfs other infectious diseases over time. At press time, COVID-19 had killed more than 5 million people; malaria has for decades killed hundreds of thousands a year, with no sign of slowing. “COVID has been a stark example of how, when you commit resources to something, you can solve it,” says Duffy. “If people could just grasp that this health crisis comes to Africa every year when it rains, maybe we could commit ourselves.”
The Gates Foundation brought worldwide attention to the problem when it launched its malaria initiative in 2005. Private philanthropy has since spent billions, largely on vaccines that target the same sporozoite-based efforts as RTS,S.
“Covid has been a stark example of how, when you commit resources to something, you can solve it.”
“Half of the more than 100 vaccine candidates currently in development are based on only four antigens—the same four that have been used for the last 40 years,” says Kurtis, with obvious frustration. “They keep thinking that repackaging dirty socks is somehow going to turn into Prada shoes.” A new vaccine candidate developed by Oxford, called R21, was 77 percent effective in small-scale Phase 2 trials in Burkina Faso. But Kurtis notes that it’s also based on the same antigen as RTS,S, which showed effectiveness of more than 60 percent in initial trials before dropping dramatically in larger Phase 3 trials.
“I suspect [R21] too will be much less effective in Phase 3 trials,” says Kurtis. “They want a vaccine that will block transmission, because that’s the only way to eradicate malaria. But I have a vaccine that could keep kids from dying.”
With the necessary funding, Kurtis estimates he could produce a shot that could end malaria’s toll within five years. “I keep writing the same thing over and over, grant after grant. Every scientist feels this way, but I have a shovel-ready project,” Kurtis says. He is hopeful that the world’s experience with the COVID-19 pandemic might open people’s eyes to the suffering caused by the annual malaria epidemic in Africa. Or perhaps governments will fund more malaria research out of their own interest in stabilizing an increasingly strategic part of the world. “We will not have peace in sub-Saharan Africa,” Kurtis argues, “until we have health in sub-Saharan Africa.”
However long it takes, Kurtis clearly won’t be giving up any time soon. “I challenge students all the time, asking them, in the morning when you wake up and you’re showering, what do you think about? Whatever it is, you want that to be your job,” Kurtis says. “For me, what I am thinking about is malaria.”
Michael Blanding is an award-winning investigative reporter and bestselling author of The Map Thief.