A Crisis for Children
A letter from the Editor
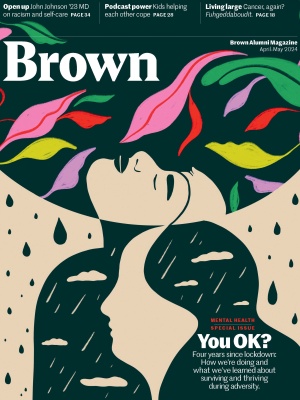
We’re not the same. In ways big and small, the pandemic changed us, and while some things are better, at least for some of us—hello, remote work—many aren’t. Foremost among them, the subject of this special issue: our mental health.
“Just living through a global health pandemic—the anxiety, the suffering—it’s not surprising mental health took a hit,” says Ashish Jha, dean of Brown’s School of Public Health and the nation’s Covid czar from 2022-2023. Then there was the isolation of lockdown, which continues for vulnerable populations; the 1.2 million Americans who died of Covid and the knock-on effects for those left behind; and the massive learning loss, on so many different measures, from school closings. Remote work is one thing—and even when it’s an option, not everyone wants it, as I’ve learned from BAM interns hungry for mentorship and connection—but remote K-12 education turned out to be something else entirely.
For adults, while political tribalism is up—and flu vaccination rates are down—“the acute impacts of anxiety and depression have gotten better, although they’re still not quite at pre-pandemic levels,” says Jha. While “pandemics have been politicized since pandemics were around,” both public health experts and we, the public, can work to try to depoliticize health decisions. “The reason to get a flu vaccine is not to show your tribal colors,” says Jha. “It’s to avoid getting really sick. The virus certainly doesn’t care.”
For young people, however, the stakes feel higher. The CDC is documenting a growing mental health crisis among them. “This is not a new problem,” Jha says—we know, for instance, that child mental health started declining as smart phones and social media became widespread. But the pandemic exacerbated it. For instance, as many parents are now acutely aware, most states don’t have enough mental health clinicians for kids. Training more takes time we don’t have. “As long as we see this as a problem to solve one patient at a time, we’re not going to get anywhere,” argues Jha. Enter public health. Population-based ideas such as school-based mental health screening get pushback—schools may not want to identify problems they don’t have the resources to solve—but hold enormous potential. “Right now everyone’s trying to see a psychiatrist,” Jha says. But only the most seriously ill kids need one; others could see a social worker or even use one of the app-based interventions you’ll find in these pages. “We could take the services we have,” Jha says, “and use them more efficiently.”
Brown is partnering with Providence public schools and medical institutions to identify real-world solutions. Doctors, educators, and public health experts will need to sit down together to figure out what’s working. “I am optimistic that if we take a public health approach, we can make serious progress,” Jha says. “But we’ve got to put our arms around it.”